A new and frightening threat that has been sweeping through many of America’s hospitals and health care facilities has been highlighted by the Centers for Disease Control and Prevention recently.
It’s called Candida auris and, while it’s an old and familiar species of fungus to health care providers, the highly common pathogen has a new and vicious edge.
It has become antibiotic resistant.
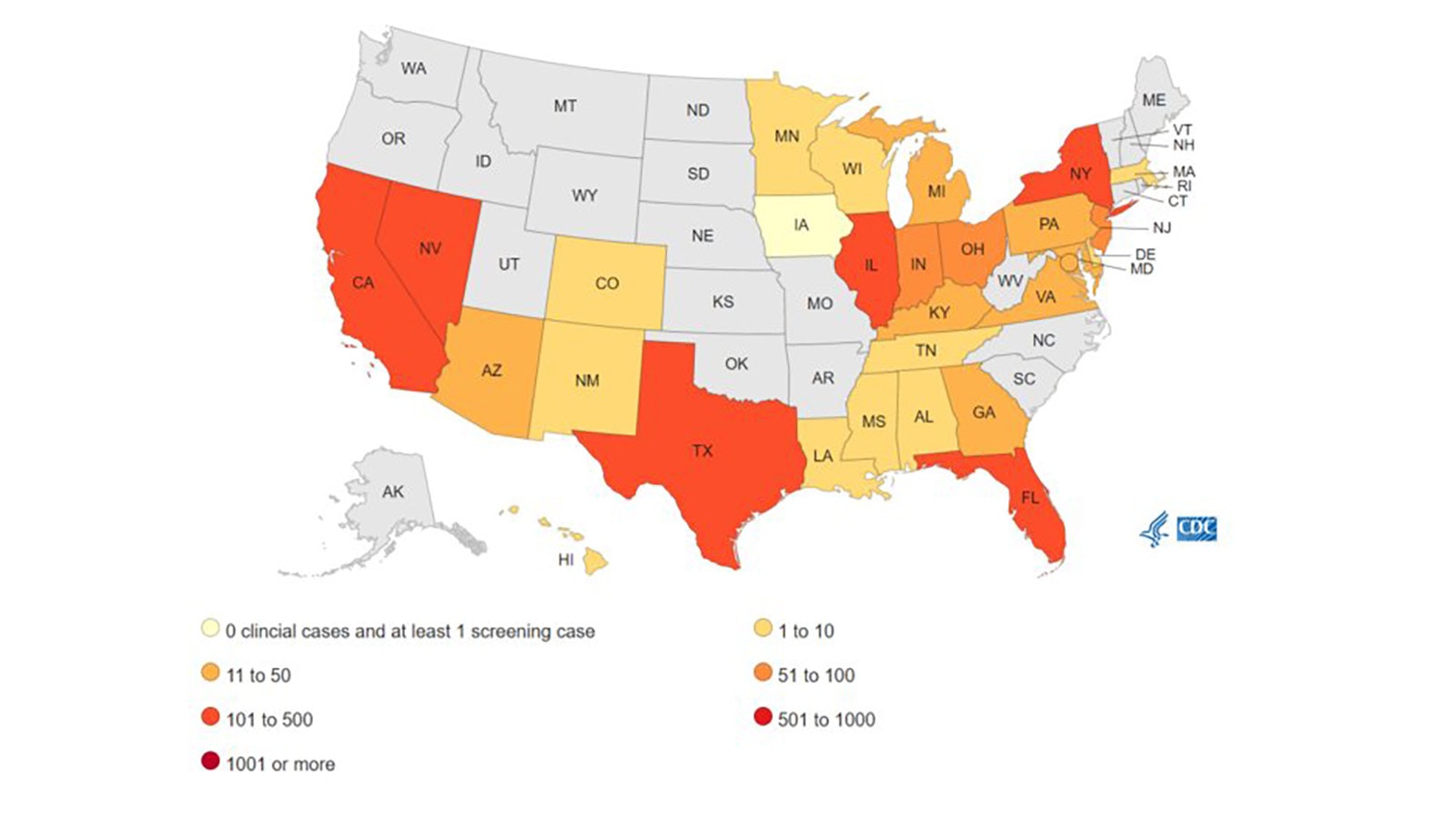
The Cowboy State, for now, has avoided any confirmed cases of the life-threatening fungus, according to the Wyoming Health Department. The presence of antibiotic resistant C. auris has been a reportable pathogen since 2018, and Wyoming has so far not had any recorded instances.
The state’s neighbor to the south, Colorado, though, has reported at least one clinical case in the last 12 months, according to CDC data.

Rapid Rise
The threat from antibiotic resistant C. auris was first reported in 2016, but its most rapid rise happened more recently during the COVID-19 pandemic from 2020-2021, according to a study published this week in the Annals of Internal Medicine.
According to the study, cases reported by medical facilities tripled from 2020 to 2021, rising to 4,041.
Seventeen new states reported their first cases of C. auris from 2019 to 2021. In that same time frame, the number of cases successfully causing infections tripled, rising from 476 to 1,471.
The reasons for this significant increase have several causes, the CDC says, including poor general infection and prevention controls in health care facilities.
But facilities these days are also more on the look-out for such cases. Many have enhanced their efforts to spot them before infections occur since the problem is easier to prevent than cure. This includes screening to see if someone has the resistant variety of fungus somewhere on their body, without infection or symptoms.
C. auris is not typically a threat to those who are healthy. Those most at risk are people who are very sick or immunocompromised, who have invasive medical devices, and those who have long and frequent stays in health care facilities.
Scary-Sounding Fungus Is Actually A Yeast
C. auris is a variety of yeast that is extremely common throughout the world, according to Wyoming University fungi expert Steve Miller.
“It’s not new. It’s been around for quite a while,” he told Cowboy State Daily. “It’s a different species than the one that causes vaginal yeast infection. What happens is that (C. auris) is really common in the air filtration systems in hospitals.”
Once C. auris gets into an air filtration system it can be almost impossible to eliminate. That’s forced some hospitals to simply close down, Miller said.
“People who go into the hospital and have surgeries and things like that, and especially immunocompromised people — how many diabetics do we have in the world these days, and how many people are living with transplants that have lowered immune systems simply because they have to take pills to keep their organ from being rejected?” Miller said.
“So, you just do all of the math and there’s a huge number of immunocompromised people in the world,” he added. “And so, in a lot of ways, the hospital becomes the worst place (for them) to go.”
Why Fungi Are So Hard To Kill
Fungi are genetically closer to humans than insects or plants, which makes treating them a new level of difficult.
Fungi, like human cells, are eukaryotic — having a nucleus — while bacteria are mainly prokaryotic, or have no nucleus.
Antibiotics that attack prokaryotes don’t tend to attack eukaryotic human cells. That helps to specifically target medicines just to the bacteria in question.
But “fungi have functioning nuclei — all of the pieces and parts that humans have, basically — so there’s not a good way to kill those,” Miller said.
That makes finding a killing agent specific to fungi difficult, and that’s why there are so few drugs in the medical toolbox for them.
Rising Resistance
Fungi, like prokaryotic bacteria, can develop resistance if every cell is not eradicated during an infection.
Those few cells that survive are that much more able to fend off future antibiotics and, over time, quickly become harder and harder to kill.
Prescribing “just-in-case” medicines for viruses — which are not affected by antibiotics anyway — has contributed to a rise in antibiotic resistance, as has the all-too-common trend where people, when feeling better, fail to take all their prescribed course of medicine. That leaves behind survivors that replicate and spread anew.
“That’s what’s happened with this Candida species,” Miller said. “We went from having, you know, (an) easy to kill fungus in the human body to having practically no way to kill this. So, this gets really serious when you get an infection like that.”
Another attribute that makes antibiotic-resistant bacteria particularly difficult to control is their ability to exude genetic information into the environment that can then be picked up by non-related, non-resistant species.
This has led to some novel ideas of controlling hard-to-kill bacteria and fungal species.
One example Miller offered is the deliberate infection of chestnut trees with a less aggressive strain of a virus that’s been killing out chestnut trees.
The trees are still infected, but with a less aggressive strain that’s — for now at least — outcompeting the more deadly version.
Things To Know
• Candida auris can cause bloodstream infections leading to death, particularly in hospital and nursing home patients with serious medical problems.
• The symptoms can be difficult to spot, particularly since those who catch it often have other ailments that can mask the symptoms.
• Fever and chills that don’t improve after antibiotic treatment for a suspected bacterial infection are among the most common symptoms.
• C. auris can be readily misidentified, leading to the wrong treatment. Specialized laboratory technology is required to properly identify this pathogen.
• C. auris spreads through physical contact with affected patients, contaminated surfaces or equipment.
• Good hand hygiene and surface cleaning is crucial. The yeast can live on surfaces for weeks.
• Always clean hands with sanitizer or soap and water before and after touching someone with a suspected case of C. auris.
• Clean surfaces with a disinfectant that is rated for use against this specific pathogen.